The Optional Second Booster
Last week the FDA permitted the administration of second COVID booster doses (meaning fourth vaccine doses) to people 50 and over. The CDC followed suit by releasing a statement highlighting the option without actually endorsing it. “Boosters are safe, and people over the age of 50 can now get an additional booster 4 months after their prior dose to increase their protection further.” Can, not should, not even are encouraged to. Even Cedars-Sinai, which required a booster dose for everyone on their medical staff, is not requiring a second booster. Why the unenthusiastic response? And more importantly, how does this weigh on whether you should get a second booster?
The main reason that the second booster isn’t widely recommended is the uncertainty of its benefit. Compare the evidence for a second booster to the evidence for the initial vaccine doses. Both the Pfizer and Moderna vaccines proved their effectiveness in randomized trials enrolling tens of thousands of patients. That means patients were randomly assigned to receive the vaccine or a placebo. They were then followed to see how many in each group became infected. That’s the most reliable way of determining the effectiveness and safety of an intervention. Every other way is susceptible to influence by biases or spurious associations.
Compared to that, the data on second boosters is very weak tea. On January 2, 2022, Israel began offering fourth doses of the Pfizer vaccine to people 60 and over and those with high-risk conditions. An unpublished study that has yet to go through peer-review compared the rates of COVID-19 infection and severe illness between people who received four doses and people eligible for a fourth dose who had only received three doses. It showed that rates of infection in the group that received a fourth dose was half of that in the group that did not, and the rate of severe illness was a quarter of the rate of those without the fourth dose. This trial was not randomized, meaning that is simply followed people who chose to get a second booster and those who chose not to. But these two groups may be very different, and the results may reflect the differences in the patients, not the effect of the second booster. For example, the Israelis who chose to get the second booster might be more health-conscious than those who didn’t and may engage in other protective behavior (distancing, avoiding indoor gatherings) more than those who didn’t. Did the authors consider these possible biases and try to control for these confounding factors? That’s very difficult to know without the paper going through peer-review.
The other study looking at second booster effectiveness is even less persuasive. It involved about 300 Israeli healthcare workers who received either the Pfizer or Moderna vaccines as fourth doses. They were compared to colleagues who had not received a fourth dose. It was also not randomized. The results were meh. Vaccine efficacy for preventing infection was 30% for the Pfizer vaccine as the fourth dose and 11% for those receiving Moderna. That tells us what we already know – the vaccines aren’t very good at preventing infection from the current more infectious variants. But did they prevent serious outcomes in this trial? “Most infected health care workers reported negligible symptoms, both in the control group and the intervention groups.” There were no serious outcomes in those who received a fourth dose or in those who didn’t. So why get a fourth dose to avoid negligible symptoms? Obviously, this is a trial in healthcare workers, who, by virtue of having jobs, would be expected to be younger and healthier than the rest of the population. So it doesn’t tell us whether older patients with serious illnesses might benefit from a second booster. But it reminds us that in many people who have had three vaccine doses, COVID is a mild disease.
A word about safety is in order. In the 50 and over age group, the vaccines, including a fourth dose, are safe. The reason that fourth doses aren’t being enthusiastically recommended is because we’re not sure they help, not because we’re worried about harm. So if you’ve already decided you want a second booster, by all means get it. The avuncular epidemiologist Michael Osterholm in his most recent podcast episode recommends that everyone eligible for the second booster get it. It won’t hurt, and it might help. So why not?
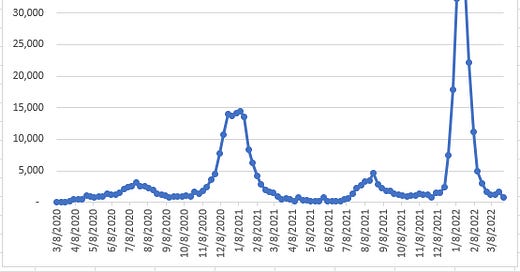
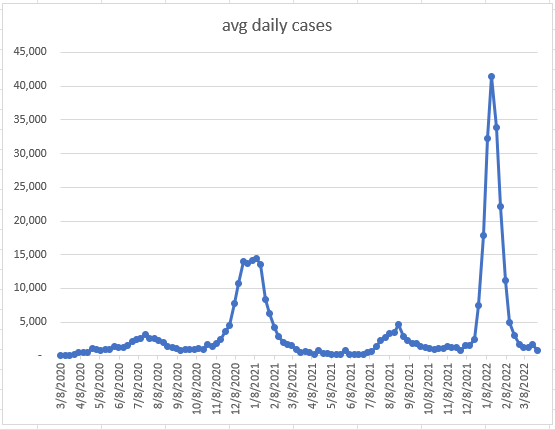
That’s sensible, but it might not help, and waiting a while might have some benefits. Both Pfizer and Moderna have large trials underway to measure the benefits of a fourth dose. Moderna is also working on a new vaccine that specifically targets omicron. So waiting a few months might clarify who benefits from further doses and who doesn’t. Case counts in LA County are as low as they were before the omicron winter surge, and thus far people who have received three vaccine doses are not being hospitalized due to COVID. COVID is still a life-threatening disease only for the unvaccinated. So there’s little risk in waiting a month or two to see if the next surge is more dangerous to vaccinated people.
So how have I been advising my patients who have sent an avalanche of emails asking whether they should get a second booster? First, I stress that this is a subjective judgment call with no solid evidence to guide us. Second, I follow an approach similar to the CDC press release that states that the second booster can increase protection which “is especially important for those 65 and older and those 50 and older with underlying medical conditions that increase their risk for severe disease from COVID-19 as they are the most likely to benefit from receiving an additional booster dose at this time.” So I’m recommending it to older patients, and those taking immunosuppressive medications, and those with serious chronic medical problems. I think everyone else can safely wait and see.
The much-ballyhooed BA.2 COVID subvariant now represents a third of COVID cases in LA County. It, like the original omicron variant, and the delta variant before it, is described as very infectious. For weeks this has led some experts to warn about a coming surge which thus far hasn’t come. Like the rooster crowing in the dark to predict the dawn, they’ll be right eventually. But what if BA.2 is even less severe than the original omicron strain? Is preventing that worth another vaccine? Maybe. I suspect that would be a subjective decision best left to each patient’s judgment. If it’s more severe, and if vaccinated and boosted people get very sick from it, I’ll be first in line for my second booster. But for now, I’ll wait.
Learn more:
CDC Recommends Additional Boosters for Certain Individuals (CDC)
Protection by 4th dose of BNT162b2 against Omicron in Israel (medRxiv)
Efficacy of a Fourth Dose of Covid-19 mRNA Vaccine against Omicron (NEJM letter to the editor)
Episode 97: This Virus Isn't Done with Us (Center for Infectious Disease Research and Policy COVID-19 podcast)
Highly Infectious BA.2 Subvariant Increasing in LA County, Accounting for 32% of All Specimens Sequenced (Los Angeles County Dept of Public Health)
Covid-19: Fourth vaccine doses—who needs them and why? (British Medical Journal)
Second Covid-19 Booster Shot Endorsed by FDA, CDC for Adults 50 and Older (WSJ)
Learning from Omicron (my most recent post about the performance of COVID vaccines during the winter omicron surge)